CAR T Cells: Engineering Patients’ Immune Cells to Treat Cancer
For years, the foundations of cancer treatment were surgery, chemotherapy, and radiation therapy. Over the last two decades, targeted therapies like imatinib (Gleevec®) and trastuzumab (Herceptin®)—drugs that target cancer cells by homing in on specific molecular changes seen primarily in those cells—have also cemented themselves as standard treatments for many cancers.
But over the past several years, immunotherapy—therapies that enlist and strengthen the power of a patient's immune system to attack tumors—has emerged as what many in the cancer community now call the "fifth pillar" of cancer treatment.
A rapidly emerging immunotherapy approach is called adoptive cell transfer (ACT): collecting and using patients' own immune cells to treat their cancer. There are several types of ACT (see "ACT: TILs, TCRs, and CARs"), but so far the one that has advanced the furthest in clinical development is called CAR T-cell therapy.
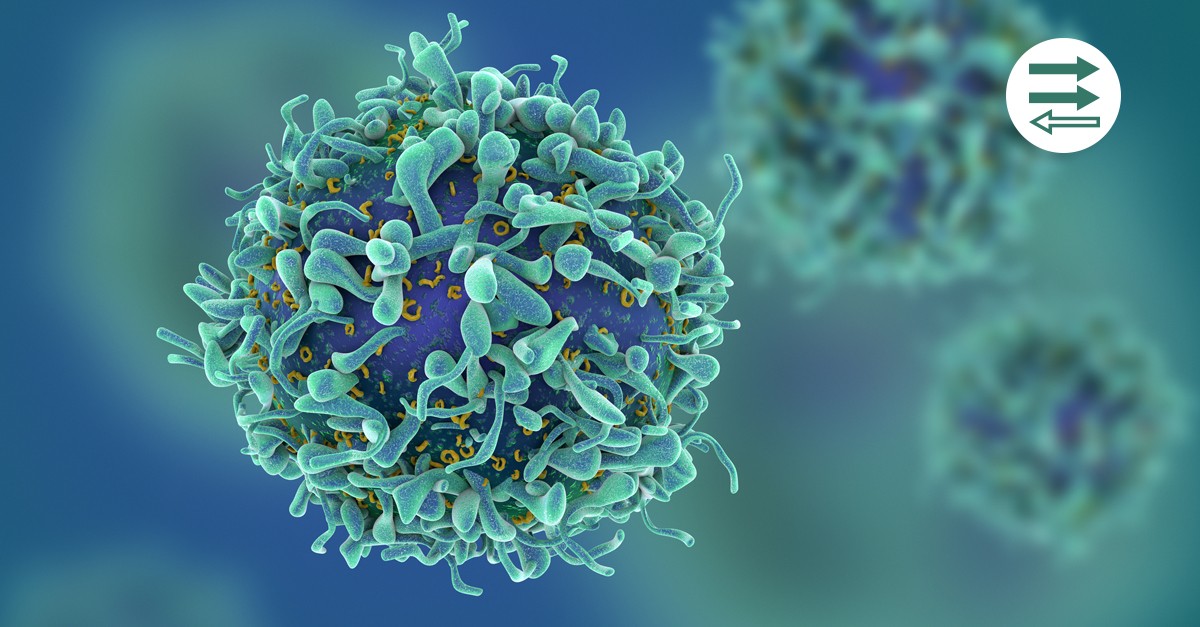
"T-cells are a type of immune cell that help the body fight infection by seeking out viruses, bacteria and parasites, and then killing them. T-cells also look for and destroy abnormal cells, such as cancer cells. Researchers have found that T-cells can be taken out of a patient's body and genetically modified to boost their ability to recognise and kill specific cancer cells.
"Researchers do this by collecting T-cells from the patient's blood, which are then modified in a laboratory to produce special structures called Chimeric Antigen Receptors (CARs) on their surface. When these CAR-T cells are given back to the patient as an infusion, the new receptors enable them to recognise specific proteins on the cancer cells and kill them.
"As CAR-T therapy is made up of living T-cells, they are able to circulate around the body just like any other blood cell. As result, CAR-T is a dynamic therapy, which reacts when it comes into contact with the target cancer cells. When this happens, the CAR-T cells release biological substances called cytokines that recruit other immune cells to join with them to kill the cancer cells.
"Research has shown that CAR-T cells can remain in the body and continue to be active for a long period of time. So unlike many other blood cancer drugs, CAR-T therapy is designed to be a one-time treatment."
Who can have CAR T-cell therapy?
"CAR-T therapy is designed for people with advanced or progressing blood cancers, who have limited treatment options open to them. It's suitable for people with certain types of blood cancer who initially responded to treatment, but then relapsed (the cancer returned). It can also help those whose blood cancer is not responding to treatment (refractory or resistant disease)."
What are the possible side effects of CAR-T therapy?
"CAR-T therapy is still very new and can cause some serious side effects, and is a major reason why this treatment is done only in hospitals that have an expert team to manage these. Sometimes, CAR-T therapy can trigger serious conditions, usually within five days of the infusion. Cytokine release syndrome can occur when immune cells activated by the treatment release an excessive amount of cytokines, resulting in a type of immune reaction similar to a severe infection.
"This can lead to flu-like symptoms, such as: high fever and/or chills; racing heart beat; drop in blood pressure; and difficulty breathing. Neurological side effects can also occur, causing the patient to experience headaches, confusion, difficulty understanding language and speaking, or stupor.
"However, in almost all cases, these side effects completely resolve within days to weeks and do not return."
What CAR-T therapy trials for blood cancer are happening in the UK?
"Bloodwise is one of a small number of organisations funding CAR-T therapy trials. I am leading University College London's Bloodwise-funded COBALTtrial, which is looking at the safety of a CAR-T therapy for people with an aggressive type non-Hodgkin lymphoma called diffuse large B cell lymphoma (DLBCL). The CAR-T therapy in this trial targets a protein called CD19 that's found on the surface of some lymphoma cells. It's a 'bridging treatment' for people with DLBCL, to get them into remission before a donor stem cell transplant."
Will CAR-T therapy cure blood cancer?
"CAR-T is an exciting new treatment which has considerably changed the outlook for some people living with blood cancer. However, it is not appropriate for all types of blood cancer, and not everyone with those cancers where it is available responds to this treatment. Why certain patients respond while others don't is not well understood, and more research is needed.
https://bloodwise.org.uk/community/what-is-car-t-therapy
https://www.cancer.gov/about-cancer/treatment/research/car-t-cells