Cancer and Gene Therapy
Gene therapy is a cancer treatment that is still in the early stages of research. [1]
Genes are coded messages that tell cells how to make proteins. Proteins are the molecules that control the way cells behave. Our genes decide what we look like and how our body works. We have many thousands of separate genes.
Genes are made of DNA and they are in the nucleus of the cell. The nucleus is the cell's control centre. Genes are grouped together to make chromosomes. We inherit half our chromosomes from our mother and half from our father.
Cancer cells are different from normal cells. They have changes (called faults or mutations) in several of their genes which make them divide too often and form a tumour. The genes that are damaged might be:
genes that encourage the cell to multiply (known as oncogenes)
genes that stop the cell multiplying (tumour suppressor genes)
genes that repair other damaged genes
Gene therapy is a type of treatment which uses genes to treat illnesses. Researchers have been developing different types of gene therapy to treat cancer.
The ideas for these new treatments have come about because we are beginning to understand how cancer cells are different from normal cells. It is still early days for this type of treatment. Some of these treatments are being looked at in clinical trials. Others can now be used for some people with types of cancer such as melanoma skin cancer.
If a gene becomes damaged, this damage is called a mutation. This can lead to a gene not functioning properly and a cell growing uncontrollably. This can eventually lead to cancer formation. Keep in mind that developing a cancer is not quite as simple as this, but requires a complex series of multiple mutations. These mutations may be caused by things like smoking, the environment, or they may be inherited. It makes sense that if we could repair these mutations, we could potentially stop a cancer from starting. The question is, how do we do this?
Researchers are testing several ways of applying gene therapy to the treatment of cancer:
Genes are coded messages that tell cells how to make proteins. Proteins are the molecules that control the way cells behave. Our genes decide what we look like and how our body works. We have many thousands of separate genes.
Genes are made of DNA and they are in the nucleus of the cell. The nucleus is the cell's control centre. Genes are grouped together to make chromosomes. We inherit half our chromosomes from our mother and half from our father.
Cancer cells are different from normal cells. They have changes (called faults or mutations) in several of their genes which make them divide too often and form a tumour. The genes that are damaged might be:
genes that encourage the cell to multiply (known as oncogenes)
genes that stop the cell multiplying (tumour suppressor genes)
genes that repair other damaged genes
Gene therapy is a type of treatment which uses genes to treat illnesses. Researchers have been developing different types of gene therapy to treat cancer.
The ideas for these new treatments have come about because we are beginning to understand how cancer cells are different from normal cells. It is still early days for this type of treatment. Some of these treatments are being looked at in clinical trials. Others can now be used for some people with types of cancer such as melanoma skin cancer.
If a gene becomes damaged, this damage is called a mutation. This can lead to a gene not functioning properly and a cell growing uncontrollably. This can eventually lead to cancer formation. Keep in mind that developing a cancer is not quite as simple as this, but requires a complex series of multiple mutations. These mutations may be caused by things like smoking, the environment, or they may be inherited. It makes sense that if we could repair these mutations, we could potentially stop a cancer from starting. The question is, how do we do this?
Researchers are testing several ways of applying gene therapy to the treatment of cancer:
- Replace missing or non-functioning genes. For example, p53 is a gene called a "tumor suppressor gene." Its job is just that: to suppress tumors from forming. Cells that are missing this gene, or have a non-functioning copy due to a mutation, may be "fixed" by adding functioning copies of p53 to the cell.
- Oncogenes are mutated genes that are capable of causing either development of a new cancer, or the spread of an existing cancer (metastasis). By stopping the function of these genes, the cancer and/or its spread may be stopped.
- Use the body's own immune system by inserting genes into cancer cells that then trigger the body to attack the cancer cells as foreign invaders.
- Insert genes into cancer cells to make them more susceptible to or prevent resistance to chemotherapy, radiation therapy, or hormone therapies.
- Create "suicide genes" that can enter cancer cells and cause them to self-destruct.
- Cancers require a blood supply to grow and survive, and they form their own blood vessels to accomplish this. Genes can be used to prevent these blood vessels from forming, thus starving the tumor to death (also called anti-angiogenesis).
- Use genes to protect healthy cells from the side effects of therapy, allowing higher doses of chemotherapy and radiation to be given.
How is gene therapy given?
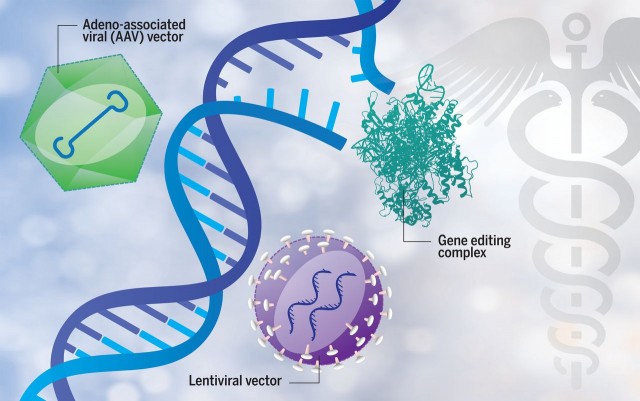
Gene delivery is one of the biggest challenges to successful gene therapy. You can imagine it would be hard to actually inject these genes into the tiny cells, so a carrier, or a "vector," is used to accomplish this. Typically, viruses are used as the vectors. The virus vector must be genetically altered to carry human DNA. These viruses are like those that cause the common cold, only they are "deactivated" so that they will not cause the patient to actually get the cold. [2]
Despite recent advances in treatment and increasing activity in the discovery of targeted immunotherapy, pancreatic ductal adenocarcinoma (PDA) remains the fourth most common cause of cancer-related deaths in the US.1 Its incidence has increased since 1999, but mortality rates have remained largely unchanged.2 With recent developments in effective immunotherapy against other previously difficult-to-treat malignancies such as melanoma and non-small cell lung cancer, there has been a growing interest in understanding fully the PDA immune microenvironment, and more specifically, how normal T-cell programming mechanisms are perturbed in this setting.[3]
[1] https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/gene-therapy
[2] https://www.oncolink.org/cancer-treatment/immunotherapy/what-is-gene-therapy
[3] https://www.nature.com/cgt/
Gene delivery is one of the biggest challenges to successful gene therapy. You can imagine it would be hard to actually inject these genes into the tiny cells, so a carrier, or a "vector," is used to accomplish this. Typically, viruses are used as the vectors. The virus vector must be genetically altered to carry human DNA. These viruses are like those that cause the common cold, only they are "deactivated" so that they will not cause the patient to actually get the cold. [2]
Despite recent advances in treatment and increasing activity in the discovery of targeted immunotherapy, pancreatic ductal adenocarcinoma (PDA) remains the fourth most common cause of cancer-related deaths in the US.1 Its incidence has increased since 1999, but mortality rates have remained largely unchanged.2 With recent developments in effective immunotherapy against other previously difficult-to-treat malignancies such as melanoma and non-small cell lung cancer, there has been a growing interest in understanding fully the PDA immune microenvironment, and more specifically, how normal T-cell programming mechanisms are perturbed in this setting.[3]
[1] https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/gene-therapy
[2] https://www.oncolink.org/cancer-treatment/immunotherapy/what-is-gene-therapy
[3] https://www.nature.com/cgt/